Perimenopause and Mental Health
The expectations set on modern women are high. Between work life, home life, sex life, and love life, it can easily feel like there isn’t enough time or energy or motivation to do it all well- or to do any of it on some days. On top of this, there is often an unspoken societal expectation that women are to do it all while maintaining balanced composure, entirely unaffected by the tides of shifting hormones happening within our bodies.
There is a popular meme that reads “Anything you can do, I can do bleeding,” which I think aptly describes what a lot of women in their ovulating years experience and feel in their day-to-day, bleeding lives. It isn’t easy to go to work when you have debilitating cramps, or maintain patience with your kids when you’re experiencing extreme fatigue. The truth is that we aren’t magically separate from the hormones that are regulated and released by our endocrine glands and organs, and needed for a host of biological processes.
What’s also true, though, is that women today are often suffering more because of the lack of deep understanding of women’s health and women’s hormones. Did you know that perimenopause- the years leading up to menopause- can be more chaotic than menopause itself and that it can start in your mid thirties? During the perimenopause years, many women will experience the symptoms of hormone shifts, but few will understand their root cause. This article will discuss the issue of perimenopause, and what happens with hormones during this time and what strategies are available to you that will help to maintain homeostasis in the body, and address whatever symptoms you may be experiencing.
If women were equipped with the knowledge of the hormonal shifts that take place across the lifespan, and what impact these changes can potentially have on mind and body, we could alleviate and even avoid significant suffering and pain. If we learn to recognize what our baseline “normal” looks like, and it will be different from woman to woman, we will be able to more easily recognize when homeostasis is disrupted. Hopefully, talking about perimenopause will equip more women with the resources to heal and restore hormone and health balance through using simple methods such as herbs, supplements, diet, and lifestyle changes.
Hormone Primer
Hormones are chemical messengers that are regulated and released by your endocrine system. These glands and organs use hormones to control and coordinate your body's metabolism, energy level, reproduction, growth and development, and response to injury, stress, and mood.
The three key hormones in perimenopause are estrogen and other sex hormones, thyroid hormones, and stress hormones, which all interact to affect the brain and body. Key players:
Thyroid Hormones: Affect metabolism, energy, weight. Produced by thyroid.
Cortisol: Major stress hormone; regulates blood sugar, blood pressure, and immune function. Produced by adrenals.
Estrogen: Regulates menstruation, keeps women lubricated from joints to vagina. Produced by ovaries along with progesterone and testosterone.
You may be interested to learn that our body fat, or adipose tissue, is the largest endocrine organ and responsible for the storage and release of energy throughout the body. Fat tissues secrete hormones such as leptin, which regulates appetite, and adiponectin which control how you burn fat.
Estrogen’s Widespread Reach
Estrogen plays over 300 roles in the female body and can impact mood, cognitive development and functioning, and vulnerability to neurodegenerative diseases and brain damage. Not only is it responsible for secondary sex characteristics in women, such as breasts, pubic hair, and regulation of menstruation, but also estrogen plays a significant role in women’s mental health.
Estrogen can impact the amygdala which controls fear and anxiety responses; the medial preoptic area of the brain in charge of locomotor activity; the cerebellum in charge of cognitive development and tumor susceptibility; and the reward pathways of the brain which can make us susceptible to addiction.
Specific to women’s mental health, estrogen has the capacity to increase serotonin and the number of serotonin receptors in the brain. It can also modify the production and effects of endorphins - the brain’s “feel good chemicals.”
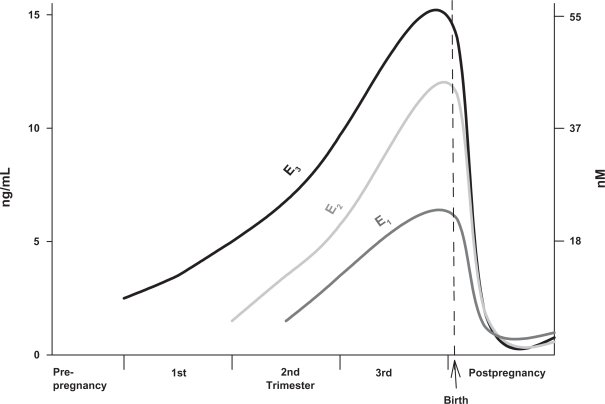
This graph illustrates the steady rise of estrogen throughout a woman’s pregnancy, rising more steeply in the third trimester before dropping sharply directly following delivery.
Source: (Watson, 2013); https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2971739/
Studies have proven that there are sex based differences in disease, with women experiencing age and pregnancy specific diseases as well as menstrual phase- dependent mood disorders. Women’s addiction rates may be affected by hormonal shifts which can increase drug addiction vulnerability. Crises in individuals with bipolar disorder and schizophrenia can sometimes also be linked directly to hormonal fluctuations associated with the menstrual cycle, particularly during the perimenopausal years when estrogen levels are more erratic.
The hormone fluctuations during perimenopause, can contribute to the onset of mood disorders. Phase dependent mood disorders are linked directly to fluctuations in hormones during the menstruation cycle. For example, depression is more common among women and especially during periods of fluctuating estrogen levels. Post partum depression is similarly associated with a sharp decline in estrogen levels following delivery.
What’s Normal?
The truth is that every woman’s baseline “normal” is different when it comes to hormone levels and the impact that they have on the mind and body. What is true for everyone with female reproductive organs, though, is that the levels of hormones produced within the body will change throughout the 28 day menstruation cycle and throughout the lifespan.
Below is an infographic that displays just how variable the hormone levels are at any given point during the menstruation cycle. Estrogen, for example, is found in its highest levels right before ovulation - its rising levels signal to the ovary that it is time to release another egg. After ovulation, estrogen levels drop just as quickly and remain constant throughout the rest of the cycle. Progesterone, on the other hand, is dominant from ovulation (day 14) until day 28, during this time progesterone triggers an increase in magnesium, zinc, and vitamin B6 levels and a drop in our body’s copper stores. This is because progesterone is preparing the body for the implantation of a fertilized egg into the uterus. If this does not take place, then the uterine lining is shed and your period starts.
Source: https://helloclue.com/articles/cycle-a-z/the-menstrual-cycle-more-than-just-the-period
Source: https://helloclue.com/articles/cycle-a-z/the-menstrual-cycle-more-than-just-the-period
Women who take oral contraceptive pills (OCPs), have added estrogens. The progesterone in OCPs is synthetic and does not have the same effect as the naturally occurring progesterone produced by the body. As a result the levels of zinc and magnesium will fall, not rise, during days 14-28. In addition there is a concern for excess estrogen.
Normal levels of estrogen vary from person to person and depend on where you are in your cycle. In the final years before menopause, it is more common for women to experience excess estrogen, called estrogen dominance, rather than estrogen deficiency.
Hormone imbalance
The balance between estrogen and progesterone is very important. Balance is a major theme in Holistic, Integrative and Traditional Medicine practices. Balance leads to health and imbalance leads to symptoms and disorders.
Unfortunately, often in western medicine, only the symptoms are treated and the root cause of the imbalance remains unknown. Integrative medicine, holistic medicine and functional medicine seek the root causes of disorders and that understanding then guides treatment.
When estrogen becomes dominant and progesterone levels are low, balance is lost. The following is a list of symptoms that may point towards estrogen dominance:
Anxiety
Depression
Fat gain
Fatigue
Foggy thinking
Headaches
Insomnia
Irritability
PMS
Thyroid dysfunction
Uterine Fibroids
Breast Cancer
Signs of Low Progesterone:
PMS
Insomnia
Painful breasts
Weight gain
Headaches
Anxiety
infertility
You'll notice that PMS is on this list - that’s right, PMS is a result of hormone imbalance. 90% of women report having “unpleasant side effects” before their period starts, and 20-40% report experiencing PMS. Symptoms of PMS include emotional disturbance - anger, irritability, anxiety, social withdrawal - as well as physical discomfort such as breast tenderness, bloating, and swelling in the arms and legs.
When PMS begins to disrupt your ability to function day-to-day, a diagnosis of PMDD may be made. PMDD is an extreme form of PMS experienced by 3-9% of women. These women may be more sensitive to the change in estrogen levels, although more research is needed to understand why or how this may be the case. It is believed that estrogen communicates with the part of the brain responsible for regulating emotions.
During the 10 years leading up to menopause, estrogen levels become more erratic and unpredictable. Up to 10% of women experience depression during perimenopause, and unstable estrogen levels may play a role in increasing the risk for depression. Some studies show that an estrogen patch can improve depression in this population, though more study is needed to confirm these findings.
According to Dr. Sara Gottfried, author of The Hormone Cure, experiencing five or more of the following symptoms consistently is a good indicator that you have entered perimenopause:
Feeling less jolly about doing day to day chores
Preference for social isolation
Need to unbutton jeans for a roll around your waist that seemed to arrive overnight?
Emotional Instability
Lack of satisfaction with exercise, since it doesn’t seem to affect your weight
General feeling of blah or reclusiveness
Problems with sleep
Waking up sweaty during the night
Crows feet and permanently furrowed brow
Lack of attention to personal grooming habits
Attitude towards children that is more ambivalent than joyful
Unpredictable menstrual period
Sudden forgetfulness when walking into a room
Continual doubting of your own instincts and insights
More frequent announcements to the family that “mom’s going to take a nap now” or “mom needs a time-out”
Preference for chocolate or a glass of wine over sex (which, frankly, may just be your lowest priority)?
A notion that antidepressant medication sounds increasingly appealing
Opinion that addressing your mood issues by giving up sugar, alcohol, and flour, taking various supplements and hormonal tweaking sounds like way too much work
The first sign of perimenopause, will likely not be an erratic period. Your ovaries will begin sending signals that a major turning point is on the horizon, and those first symptoms will involve your mood, sleep, weight, sex drive and a willingness to accommodate the people in your life, as described above.
Excess Estrogen
When and why do things go wrong? Mental fog, fatigue, weight gain, and other side effects of hormone imbalance do not have to be the norm during the perimenopause years.
Scientists are still studying the more than 300 roles estrogen plays, but they do know that estrogen has a couple mechanisms of action: it can interact with proteins and molecules on the surface of a cell, and it can impact internal cell regulation by altering gene expression. As we mentioned earlier, women are especially sensitive to hormone shifts. The interconnectedness of shifting hormones in the female body is extensive, so that any change in the level of one hormone can trigger a series of changes in other hormones, metabolism and other body functions.
According to Dr. Gottfried, there are seven root causes of excess estrogen:
Diminished ovarian reserve: Starting at about age 35 the ovaries produce up to double as much estrogen as they did during normal menstruation cycles of a woman in her early 20s. This happens when ovaries start running out of eggs and work extra hard to ovulate. Estrogen plummets at the end of perimenopause.
Cortisol Linked Estrogen Dominance: High levels of cortisol can block progesterone receptors. This can lead to estrogen dominance.
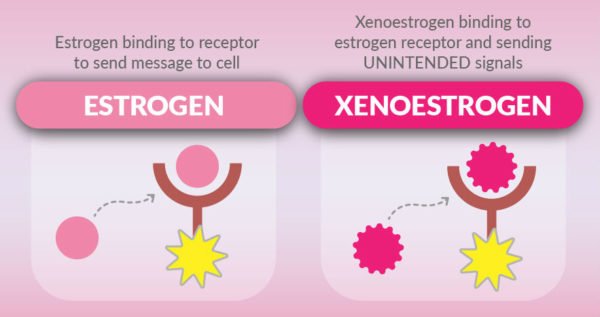
Xenoestrogens: These are chemicals that mimic estrogen and that bioaccumulate in our fat cells. They are endocrine disruptors which means they alter the regular functioning of endogenous hormones and have reproductive and developmental consequences. (More on these later.)
Obesity and Weight Gain: Fat cells produce estrogen and women who gain 20 or more pounds between 18 and middle age double their risk of postmenopausal breast cancer.
Diet: A diet high in conventionally raised red meat and refined carbs will likely lead to estrogen dominance for a few reasons. Conventional meat contains antibiotics and synthetic hormones; people who eat this kind of diet have a different gut microbiome, which may be less efficient at breaking down estrogen. In addition, refined carbs like white flour, sugar, and rice lower the levels of progesterone. Alcohol also raises estrogen and slows down fat burning.
Nutritional Deficiencies: Vitamin B12, folate, and methionine encourage production of ‘good’ estrogen, and decrease formation of ‘less good’ estrogens.
Mercury: Acts as xenoestrogen and binds to estrogen receptors in the body.
Why We Need to be Talking About Xenoestrogens
Xenoestrogens mimic endogenous estrogens, but trigger different cell responses and disrupt regular endocrine functioning.Source: https://gutdetective.com.au/xenoestrogens-root-cause-hormonal-imbalance/
We are increasingly experiencing the bioaccumulation of xenoestrogens in our fat cells. “Xeno” means stranger. These are molecules, which look like endogenous estrogens but do not behave in the same way. We take in these toxins from our surrounding environments and house them in our fat cells, though it is not clear at what threshold these xenoestrogens become toxic to the body. What is clear is that they are carcinogenic and can lead to hormonal imbalance and disrupt the regular functioning of biological or biologically equivalent estrogen.
Xenoestrogens are considered endocrine disruptors as they disrupt normal estrogen signaling in the body, and exposure at high levels is associated with a variety of reproductive, neurological, and other impairments.
The alarming thing about xenoestrogens is that they are seemingly all around us. They are found in deodorant, plastic wrap, sunscreen, the lining of canned food (even organic), and facial moisturizers, it probably isn’t possible to avoid them altogether but it is important to reduce your exposure. These compounds break down slowly and stay in the environment for extended periods of time, eventually making it into our food and water supplies.
Most common types of xenoestrogens:
BPA (bisphenol-A): found in plastic beverage bottles, canned food liners, and epoxy dental sealants.
Phthalates: industrial chemicals used in soft, flexible plastics and in PVC products
Pesticides: DDT, DDE, Dioxin
Hormones: from poultry and industry and antibiotics in animal feed
Source: https://www.meghantelpner.com/blog/xenoestrogens-what-are-they-and-where-are-they-found/
Lifestyle and nutrition approaches to healing hormone imbalance
If you think you may be dealing with a hormone imbalance or you would like to know where your hormone levels stand, consider getting your blood checked. There are simple saliva and blood tests for hormone levels. Check thyroid hormones when you get your sex hormones checked, as excess estrogen can affect thyroid function.
If you do get tested and find your hormones are out of balance, or if you are experiencing the symptoms of imbalance as described above, there are various diet and lifestyle changes that you can adopt which can drastically improve your quality of life. It is amazing how much of a difference can be made by adopting simple, intentional actions to improve hormone balance.
Nutrition/Diet Recommendations:
Reduce caffeine
Avoid xenoestrogens
Avoid conventional meat and dairy and choose grass fed and organic instead
Increase fiber in diet
Increase cruciferous vegetables or take DIM supplement
Include seaweed in diet
Maintain healthy weight
Include ground Organic Flaxseed (or prunes or fiber supplement): Increasing fiber in the diet helps to eliminate excess estrogen from the body.
You may also consider trying the following supplements which have been proven to support hormonal rebalancing.
Supplement Recommendations
Pure DIM: Plant based chemical found in cruciferous vegetables
Branded estrogen balancing blends including DIM, such as Femquil from Xymogen (contains DIM, black cohosh, chaste berry tree, vitamin B12, and other herbs and vitamins)
Progesterone Cream (optional): Progesterone is worth considering as it can be helpful. If using a cream, the dose needs to be tailored to your specific symptoms and menstrual cycle. Progesterone is also available in oral form, but this option should only be considered if the cream is ineffective, as it has been associated with more significant side effects.
Melatonin (optional)
Turmeric (optional)
It is also a good idea to limit your exposure to xenoestrogens. Try adopting a few of the following guidelines outlined by Dr. Sara Gottfried:
Reduce canned food (BPA)
Eat from glass, stainless steel, ceramic containers
Do not microwave plastic containers if you must use them
Look for all natural alternatives to cosmetics, nail polish, deodorants, and lotions
Remove your shoes when you walk into the house - you carry in with you endocrine disruptors on the bottoms of your shoes!
Buy shoes made from natural materials (chemicals in shoes made from plastics can leach into sweaty feet)
Wear organic cotton (conventional cotton has pesticides)
Use organic sheets and mattresses
Apart from these diet and lifestyle recommendations, treatment of hormonal imbalance with estrogen has been proven effective in relieving some symptoms of PPD, and in reversing depression. Hormone Replacement Therapy HRT needs to be carefully considered due to significant risks. Diet and lifestyle interventions should be adopted before pursuing hormone therapy because the risks and unknowns associated with the latter are higher. Any hormone regimen should deliver the most effective estrogens, over the lowest possible effective doses, with the most effective scheduling and fewest side effects.
We still have a lot to learn about the complicated signaling pathways and mechanisms of estrogen in our bodies. Once we understand more about estrogen’s role in the body, as well as the impact of xenoestrogens, we will be able to better prescribe medical interventions to address imbalances.
Final Thoughts
Between perimenopause, estrogen imbalance, xenoestrogens, and recommendations for diet and lifestyle, this may feel like a lot of information to absorb all at once. Perhaps the most important thing to remember is that as women, we are constantly bathed in hormonal soup of varying components. Hormone levels are impacted by a host of factors including stress, diet, weight, and exposure to neuroendocrine disruptors (xenoestrogens), and as a result hormone balance is challenging to maintain.
From PMS, to fibroids, depression, and anxiety, the side effects of hormone imbalance are real, and especially felt among women in perimenopause. If you are perimenopausal and find yourself experiencing brain fog, intense fatigue, lack of motivation, low libido, or mysterious weight gain consider meeting with an integrative practitioner to evaluate your hormones and how they are impacting your physical and mental health.
It is possible to live an invigorated, inspired, sharp, and social life during the perimenopause years, so do not compromise! You deserve to feel your best in body and mind, and an integrative approach to hormone wellness will go a long way in getting you there.
References:
Gottfried, Sara. (2013). The Hormone Cure. New York, NY. Scribner.