Integrative Treatment Options for Seasonal Affective Disorder (SAD)
Cooler temperatures can drain you of your energy and affect your mood, particularly in the fall and winter months following daylight savings time. Many interpret these feelings as a case of the “winter blues” but if they persist, the feelings could be related to a clinical condition called seasonal affective disorder (SAD).
SEASONAL AFFECTIVE DISORDER- AN OVERVIEW
According to the National Institute of Mental Health, seasonal affective disorder is a type of depression that comes and goes with the seasons. It typically starts in the late fall and early winter and resolves during the spring and summer. While depressive episodes linked to the summer can still occur, they are much less common than winter episodes of SAD.
SIGNS, SYMPTOMS, AND DIAGNOSIS
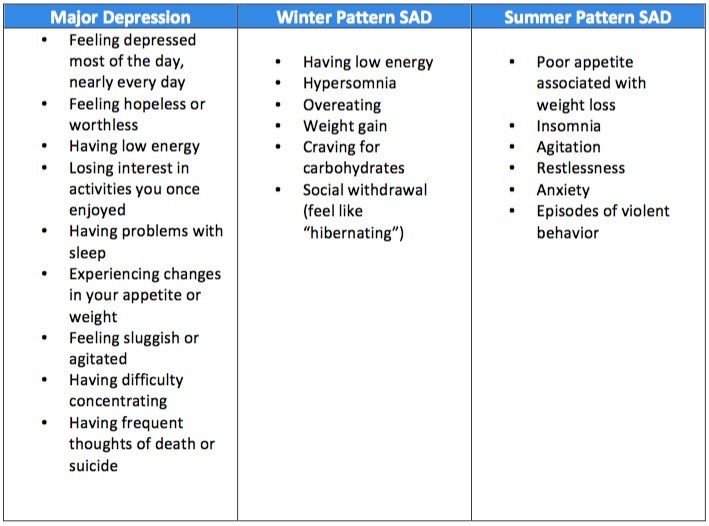
SAD is not classified as its own separate disorder, but rather a subtype of major depression marked by a recurring seasonal pattern. It shares many of the same symptoms as major depression but is distinguished by other, season - specific symptoms.
View fullsize
Depression Types and Corresponding Symptoms
Those who meet the full criteria for major depression coinciding with specific seasons (appearing in the winter or summer months) for at least two years may be diagnosed with seasonal affective disorder. Seasonal depressions must be more frequent than any non-seasonal depressions.
There are several attributes that may increase one’s risk of developing seasonal affective disorder:
Gender: Women are diagnosed with SAD four times more often than men.
Distance from the equator: Those who live further north or south of the equator may have an increased risk.
Family history: This includes those with a family history of other types of depression.
Having depression or bipolar disorder: If you have already been diagnosed with depression or bipolar disorder, your symptoms of depression may worsen with the seasons. However, it will only be diagnosed as seasonal affective disorder if your seasonal depressions are the most common.
Age: Younger adults are at higher risk for SAD than older adults. Lower rates have also been reported in children and teens.
CAUSES AND TREATMENT OPTIONS
The causes of seasonal affective disorder are currently unknown, however, research has identified several biological traits which are helping doctors to gain a better understanding of the disorder. People with SAD may:
Have difficulty regulating serotonin, one of the key neurotransmitters involved in mood.
Overproduce melatonin, the hormone which regulates sleep.
Underproduce Vitamin D, which plays an important role in a multitude of biochemical pathways in the body.
There are four main treatment options available for seasonal affective disorder:
Medication
Light Therapy
Psychotherapy
Vitamin D
MEDICATION
Selective serotonin reuptake inhibitors (or SSRIs) are the type of medications most commonly used to treat depression and anxiety. These medications work to regulate the level of serotonin in the brain--the key neurotransmitter that helps regulate mood, sleep, appetite and digestion.
Common SSRIs include Zoloft (sertraline), Prozac (fluoxetine), Celexa (citalopram), Lexapro (escitalopram) and Paxil (paroxetine). In 2006, an antidepressant called bupropion (Wellbutrin) was also approved for use by the FDA to treat seasonal affective disorder.
Advances in medical research have led to the refinement of SSRIs, improving their ability to target specific subtypes of serotonin receptors. This has resulted in a reduction of side effects, though as with other medications, side effects are still possible.
The benefits of SSRIs are not immediately felt as it may take two to four weeks before changes in neurotransmitter receptors takes place. While all of the medications listed can be considered for treatment of SAD. Bupropion is the only FDA approved preventative medication for seasonal affective disorder. Bupropion can be started in September to November and continued for four to six months to prevent SAD.
VITAMIN D SUPPLEMENTATION
Scientists believe that one of the root causes of seasonal affective disorder is vitamin D deficiency (VDD). Worldwide, it is estimated that one billion people have VDD, and this is very concerning because VDD is increasingly being implicated in diseases like type II diabetes, colon cancer, and autoimmune disease. Those who are vitamin D deficient may also be twice as likely to be diagnosed with schizophrenia.
Unlike other vitamins, vitamin D functions like a hormone in our bodies and plays a significant role in serotonin activity. As many of you are already aware, serotonin is the key neurotransmitter involved with mood, sleep, appetite and digestion. It seems reasonable then that a deficiency in vitamin D could lead to dysregulation of these processes.
Vitamin D is often called the “sunshine vitamin” because our bodies require the UV B radiation that the sun produces in order to make it. 7-dehydrocholesterol is a precursor to cholesterol found in the skin that turns into vitamin D3 upon absorbing UV B radiation (the body is magical like that!). Without UV B radiation, our bodies can’t make vitamin D3 it needs to function optimally.
Sun induced vitamin D production varies based on the season, distance from equator, air quality, and time spent outdoors. In the winter, vitamin D levels may be suboptimal as a result of a shorter exposure time to sunlight, and interestingly, people who live further from the equator in either direction (north or south) are at an increased risk of developing seasonal affective disorder.
A 2013 meta-analysis found that low vitamin D levels were associated with depression. There has been less research focused on seasonal affective disorder in particular, but one randomized controlled trial comparing vitamin D supplementation to light therapy had promising results. It showed that after one month of vitamin D supplementation, participants saw significant improvement across all items on the mood questionnaire used for the study. The outcomes correlated with a rise in vitamin D blood levels of 74%.
IS VITAMIN D SUPPLEMENTATION RIGHT FOR YOU?
Optimal vitamin D levels are considered between 33 and 80 ng/mL. Those with less than 33 ng/mL are considered to be insufficient in D, less than 20 ng/mL is deficient and, and less than 10 ng/mL severely deficient.
Your body naturally makes vitamin D from cholesterol when your skin is exposed to sunlight. While certain foods such as fatty fish and fortified dairy products are known to contain some vitamin D, it is difficult to get the recommended daily intake from diet alone. Officially the recommended daily intake for the average adult ranges from 400-800 IU (or 10-20 mcg), but that may not be enough to maintain normal levels of vitamin D. Based on the level of vitamin D in your blood, the recommended daily intake may be even higher (1,000-2,000 IU), and if you are deficient you may need even more than that to increase your vitamin D levels.
There are several ways to help increase your levels of vitamin D including diet, safe sun exposure, and supplements. However, working to increase your level is best done at the recommendation and under the supervision of a licensed medical professional so that you can monitor blood levels of vitamin D to achieve levels in the optimal range. Since vitamin D is fat soluble it is possible to overdose on vitamin D, so it is important to not overdo supplementation.
LIGHT THERAPY
For those who are averse to taking medications or supplements, or who are looking for a complementary treatment, light therapy may be a great option.
Light therapy involves sitting close to a light box emitting bright, artificial light for at least 30 minutes per day, preferably in the morning soon after waking up. This kind of therapy has been scientifically proven to be as effective as antidepressant medications in reducing the winter depressive symptoms of seasonal affective disorder (SAD). Light boxes for treatment of SAD would ideally provide 10,000 lux (the lux is the unit of measurement for light). For comparison, light intensity on a sunny day is 50,000 lux.
In one study, 332 patients from 14 research centers were studied over a period of 5 years. Overall, those who were exposed to 2500-lux intensity light for at least two hours each day for a period of one week saw a depression score reduction of 50% or more on the Hamilton Depression Rating Scale (HAM-D).
Though proven to be effective, it’s important to note that the National Institute of Mental Health reports that nearly half of all people with seasonal affective disorder don’t see improvement from light therapy alone. In these cases, it is best used as a supplement to other treatment methods.
WHAT KIND OF LIGHT DO I USE?
While there have been many products developed over the last several decades corresponding to advances in research on SAD, there is more to light therapy than simply switching out the bulbs in your home or office.
Research has shown that human circadian rhythms are more sensitive to short wavelength light. As a result, light treatment devices that use efficient light-emitting diodes (LEDs), whose output is relatively concentrated in short wavelengths, may help increase the effectiveness of light therapy. However, some wavelengths of light can be hazardous to your eyes or skin, so it’s important to consult with a healthcare professional before beginning light therapy. There are a few reputable companies making light boxes for the treatment of SAD that are easily accessible on Amazon and other sources.
HOW MUCH LIGHT EXPOSURE IS ENOUGH?
The right “dose” of light exposure is dependent on a variety of factors including an individuals needs, lifestyle, time of day, the distance between the user and the device, and the intensity and wavelengths of light that are emitted from the device. Too much light can have a similar effect as consuming too much caffeine and leave a user feeling “wired.” Not enough exposure, and you may feel as though the treatment is ineffective.
It’s important to consult with a healthcare professional that is experienced in administering and monitoring the effects of light therapy. They can help recommend an appropriate light type and illumination “dose” to offset the symptoms of seasonal affective disorder, particularly when cold weather or fewer daylight hours make exposure to outdoor sunlight difficult.
Keep in mind, light therapy requires consistent use over time. It is a commitment that often involves a minimum of 30-60 minutes per day until the season changes and your exposure to natural sunlight increases. If you get a light box which provides 10,000 lux then the daily dose may be 30 min a day if you sit with your face within 12 inches of the light or 60 min a day if you sit with your face 18 inches from the light. Ideally you use your light first thing in the morning. For bipolar depression the recommendations are somewhat different and more caution is needed to avoid triggering a hypomania or a mania and mid-day timing of light therapy around 2pm may be better.
WHEN TO SEEK HELP
If you are experiencing the symptoms of major depression and/or the season-specific depression symptoms, it is important to consult with a medical professional. If you are in Brooklyn, our care team can work with you to find the most effective treatment option for your individual needs. This may include supplements or a combination of supplements, psychotherapy, light therapy, and medication. Contact us at (212) 621-7770 and our intake coordinator will work with you to match you with the right clinician for your needs.